What are short-chain fatty acids?
Short-chain fatty acids (SCFAs) are metabolites resulting from the fermentation of dietary fibers and resistant starch by the anaerobic microbiota in the large intestine of the gastrointestinal (GI) tract. They are also known as postbiotics. SCFAs are saturated aliphatic organic acids consisting of one to six carbons, with acetate (two carbons), propionate (three carbons), and butyrate (four carbons) being the most abundant. In the large intestine, the majority of the SCFAs are rapidly absorbed by the epithelial cells lining the colon.
SCFAs provide a connection between the microbiota, redox signaling, and host metabolism and may play a beneficial role in human health due to their metabolic and signaling properties. Their functions have been attributed to their aliphatic tail length and the activation of specific membrane receptors. SCFAs may play a supportive role in healthy oxidative and mitochondrial stress response, energy metabolism, healthy aging, and in chronic diseases such as diabetes, metabolic syndrome, neuropathologies, and cancer.
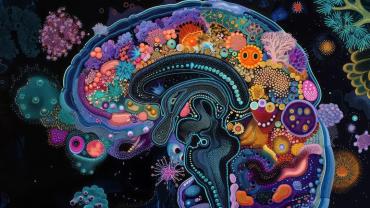
How do SCFAs support the gut-brain axis?
The gut microbiome consists of 1013 to 1014 microorganisms, weighing about 1 kg in an adult. In the human body, there are more gut microorganisms than the number of human cells. It is a complex and dynamic system that may play a role in immune function and tolerance, fiber metabolism, drug metabolism, maintaining the intestinal barrier, and synthesizing certain vitamins, amino acids, and SCFAs. The microbiome composition of each individual is unique and may be influenced by genetics, physiology, colonization history, diet, medications, and environmental factors.
The gut-brain axis is a complex network for bidirectional communication between the central nervous system and the enteric nervous system, an extensive neural network that traverses the walls of the GI tract. The gut microbiome and its metabolites communicate with the CNS through neural, endocrine, and immune pathways to ensure optimal physiological functions. More specifically, the gut microbiota may communicate with the CNS by producing neurologically active substances and supporting the hypothalamic-pituitary-adrenal axis.
The imbalance between beneficial and pathogenic bacteria in the gut microbiome, known as intestinal dysbiosis, may lead to a pro-inflammatory state by disrupting the host immune homeostasis and intestinal barrier function. Intestinal dysbiosis may also lead to an excessive release of lipopolysaccharides, which are immunostimulatory endotoxins produced by gram-negative bacteria. In the presence of dysbiosis and a compromised intestinal barrier function, LPS and other bacterial products may enter the blood-brain barrier, which may induce chronic inflammation and damage the BBB. An impaired BBB may allow the transfer of potentially harmful bacterial products, like LPS and activated leukocytes, into the brain, resulting in neuroinflammation. Chronic neuroinflammation may be associated with neurodegenerative symptoms, such as anxiety, depression, impaired locomotor function, muscle weakness, paralysis, learning difficulties, memory loss, inability to focus, and dementia.
SCFAs, one of the main bioactive metabolites of the gut microbiome, may play a protective role in neuropsychiatric disorders. They are ligands for free fatty acid receptors 2 and 3 (FFAR2/3), which are widespread in enteroendocrine, immune, and neural cells. The majority of SCFAs are taken up by colonocytes and used to maintain intestinal barrier function, which hinders LPS and other harmful bacterial products from entering the BBB. In addition, SCFAs may play a regulatory role in the transfer of nutrients and molecules involved in the maintenance of the BBB integrity and thus influence brain development and CNS homeostasis. SCFAs may also mediate several neurological processes through the modulation of the immune system, HPA axis, tryptophan metabolism, and neurotransmitter synthesis.
One animal model study found that SCFAs may play a role in ameliorating depressive behavior by mitigating hippocampal neurogenesis decline, BBB damage, and neuroinflammation. A randomized controlled trial (n = 66) found that SCFAs may have the potential to attenuate the cortisol response to psychosocial stress and fear in healthy men, suggesting that SFCAs may play a role in modulating the HPA axis.
The role of polyphenols in microbiome diversity and SCFAs formation
Polyphenols are compounds found primarily in fruit, vegetables, and spices, such as berries, pomegranate, broccoli, grapes, red wine, cocoa, cinnamon, and olive oil. They may play a supportive role in antioxidative status and healthy inflammatory, immune, and insulin responses. Depending on the number of phenol rings and on the structural elements that bind these rings together, polyphenols can be categorized into several groups: flavonoids (e.g., quercetin), phenolic acids (e.g., curcumin and caffeic acid), lignans (e.g., sesamin and pinoresinol), and stilbenes (e.g., resveratrol). Due to their partial digestion by the host and the capacity to be fermented by intestinal microorganisms, polyphenols can be categorized as prebiotics.
In their role as prebiotic substrates, polyphenols may have a modulatory effect on the GI microbiome and may help increase the production of SCFAs. A systematic review of the prebiotic effects of polyphenols found that their consumption may play a role in increasing the abundance of certain beneficial commensal species, such as Lactobacillus, Bifidobacterium, Akkermansia, Roseburia, and Faecalibacterium, and decreasing plasma LPS-binding protein. Furthermore, the study found that polyphenol supplementation may support the production of SCFAs, including butyrate. Another review article on the prebiotic effects of polyphenols came to similar conclusions regarding the role they may have in stimulating the proliferation of beneficial bacteria and increasing the production of their valuable metabolites, such as SCFAs. By supporting probiotic bacterial species, such as Bifidobacteria and Lactobacillaceae, polyphenols also contribute to the crowding out and reduction of pathogenic bacteria, such as Escherichia coli, Clostridium perfringens, and Helicobacter pylori.
Further research in the form of human randomized controlled clinical trials is warranted to investigate the prebiotic effect of dietary polyphenols on humans. However, currently available research provides compelling evidence that polyphenols may play a role in stimulating both the growth of beneficial microorganisms and the production of SCFAs. Supplementation with prebiotics, such as polyphenols, and postbiotics, such as butyric acid, may play a supportive role in GI and brain health.
Learn more about SCFAs and the microbiome:
Recent Review Explores Biochemical Relationship Between Gut Metabolites and Metabolic Health
The Latest on Red Grape and Gut Microbial Health
Recent Randomized Crossover Trial Explores the Role of Prebiotics in Individuals With Prediabetes
By Antonia Toupet, PhD