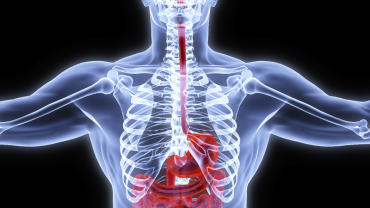
According to a new study published on May 1st UCLA researchers identified a relationship between the gut microorganisms and brain volume in those with irritable bowel syndrome (IBS).
This is the first time researchers have been able to show an association between the gut microbiota and regions of the brain involved in sensory information processing in patients with IBS. These results suggest that signals from the brain can influence the composition of gut microbes and also that the chemicals in the intestine can shape the structure of the brain.
Previous animal studies have demonstrated effects of gut microbiome on brain function and behavior as well as the influence of the brain on the composition of microbes in the gut. That being said only one human study has confirmed these findings.
Other research has demonstrated evidence for alterations of gut microbiome in people with IBS but there lacked consistency. There has been an association with structural and functional brain changes in relation to a person's history with childhood trauma and childhood trauma has also been shown to alter gut microbial composition.
In this new study researchers at UCLA collected behavioral and clinical measures stool samples and brain images from 29 adults diagnosed with IBS and 23 healthy individuals. They used DNA sequencing to quantify composition abundance and diversity of the gut microbiota. The researchers then cross-referenced these gut microbial measures with structural features of the brain.
The samples from those with IBS were clustered into two subgroups based on the composition of the microbes in the gut. One group could not be distinguished from the healthy control subjects while the other group did show differences. Those in the group with an altered gut microbiota had a greater history of early life trauma and longer duration of IBS symptoms. Both groups also displayed differences in brain structure.
The researchers stated that an analysis of an individuals gut microbiome may become a routine screening test for people with IBS in clinical practice and in the future therapies such as certain diets and probiotics may become personalized based on an individual's gut microbial profile. This is what many of us in functional medicine have been doing for the past several decades.
One may need a combination of botanicals enzymes and probiotics to optimize the gastrointestinal environment. Certain diagnostic tests may also be beneficial including stool testing as well as food antibody testing. In addition a number of studies have suggested a potential role for serum-derived bovine immunoglobulin/protein isolate (SBI) as a potential therapy for IBS.
By Michael Jurgelewicz DC DACBN DCBCN CNS