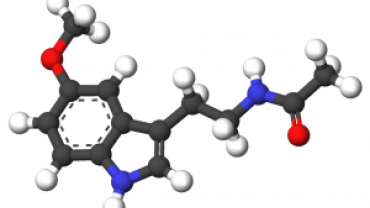
Melatonin is a neurohormone that is produced in the brain primarily by the pineal gland from the amino acid tryptophan. Its most well known functions include helping to regulate sleep and the body's circadian rhythm.
The amount of melatonin we produce is determined by how dark or light our surroundings are. Our eyes have specialized light-sensitive receptors that relay this message to a cluster of nerves in the brain called the suprachiasmatic nucleus or SCN. The SCN sets our internal biological clock (circadian rhythm) while also regulating sleep. When our surroundings are dark the SCN tells the pineal gland to produce melatonin which is thought to trigger sleep. Some melatonin is also made in the stomach and intestines.
Certain plant foods contain naturally-occurring levels of melatonin including tropical foods like bananas pineapples and oranges consumption of which can positively affect serum levels of this important hormone.
As we age like most endogenously produced hormones melatonin's production significantly declines. This may be why many elderly individuals have trouble sleeping.
On the other hand and much to the chagrin of some parents there is speculation that as children become teenagers the nightly schedule of melatonin release is delayed leading to later sleeping and waking times.
In addition to the pineal gland the gastrointestinal tract is another primary producer of melatonin possibly making it the most important source of melatonin next to the pineal. This also leads us to the question of what possible role melatonin may play in GI health and conversely its pathology. Fellow neurotransmitter serotonin which is also produced in significant amounts in the GI tract appears to have an antagonistic relationship with melatonin as they both function to enhance or modulate gastric empting GI motility and transit time. Specifically it appears that exogenous melatonin inhibits gastric motility in part by activating sympathetic neurons as well. These findings documented the relationship between serotonin and its derivative melatonin suggesting that high doses of melatonin inhibit gastric motility by interacting with serotonin receptors present on the vagal afferent fibers and inducing vago-vagal inhibitory reflexes.
It may not be surprising then that melatonin supplementation has been shown to positively impact a variety of GI disorders. Patients with gastroesophageal reflux disease or GERD are typically prescribed proton pump inhibitors (PPIs). Because the medication will decrease stomach acidity a common side effect is reduced mineral and vitamin absorption and ultimately deficiency with long term use.
Treatment of GERD with melatonin however works on a different mechanism of action and according to the study below compared the antiulcer and gastro duodenal protective mechanism of famotidine omeprazole and melatonin and their results revealed that the three drugs have gastroduodenal protective action but famotidine and omeprazole have lowering effects on gastric acidity (antisecrotory activity) whereas melatonin has no effect on this parameter but famotidine and omeprazole were not efficient as antioxidant as melatonin.
Research has established that melatonin displays antioxidation and anti-inflammatory characteristics. By modulating the production of TNF-alpha IL-1 and IL-8 in animal models of gastric ulcerations and colitis melatonin demonstrates tissue protective properties.
Like its precursor 5-HTP melatonin in several studies has been shown to also decrease the symptoms surrounding irritable bowel syndrome as well.
While part 1 of this blog deals primarily with melatonin's positive effect on gastrointestinal disorders part 2 will elucidate many more clinically relevant uses for this interesting and possibly underutilized hormone.
Michael Fuhrman D.C.