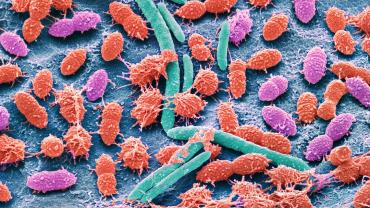
According to recent research, the incidence of pathologies associated with the allergic response is increasing. Evidence suggests a potential link between gut microbial integrity and allergic diseases. This may be due to the role the gastrointestinal microbiome plays in the development and function of the immune system. A recent review article by Chernikova and colleagues has investigated the connection between food allergy and the gut microbiome.
The body’s response to allergens is a complex process that involves immune and inflammatory pathways. It often manifests as conditions such as allergic rhinitis, atopic dermatitis, and food allergies, and it is estimated to affect more than 20% of the general population. Evidence suggests that the gut microbiome may be critical to food allergy modulation.
An animal study indicated that germ-free mice did not achieve food allergen tolerance. This suggests that the gut microbiota play a key role in the body’s immune response to food allergens. Chernikova and colleagues postulate that this may be due to the production of short-chain fatty acids (SCFAs), such as butyrate and the induction of regulatory T-cells and interleukin (IL)-22 production. Increased IL-22 production may help support improvements in epithelial permeability.
The SCFAs propionate binds to the G-protein coupled receptor GPR41, which helps support antigen-presenting cell precursors in the colonic epithelium. Another SCFA-binding receptor, GPR43, has been shown in animal studies to help support the differentiation of regulatory T-cells. In GPR32 knock-out models, researchers observed higher levels of food allergy susceptibility. Clinical studies have also correlated the incidence of allergic symptoms with low levels of SCFAs during childhood.
Clinical trials have been exploring the potential for microbiome therapeutics to support the body’s response to allergic reactions. Some studies indicate that the presence of Bifidobacterium longum and certain Prevotella species during pregnancy have been linked to the potential prevention of certain qualities related to the development of food allergies during childhood. The administration of probiotics, such as Lactobacillus rhamosus, has been correlated with a higher level of achieved allergenic tolerance to non-immunoglobulin E cow’s milk in some infant studies. Improvements in colic and symptoms related to skin or food allergies were observed in children after the administration of Lactobacillus reuteri. In adult populations, decreases in eczema severity have been observed after the administration of certain probiotic strains.
More research is needed, particularly in the clinical setting, with larger treatment populations and more varied microbiome considerations. However, research indicates a link between gut microbial health and a healthy response to certain allergens. Evidence also suggests that certain microbiome therapeutics may help support aspects of immune health.
By Colleen Ambrose, ND, MAT