The link between mood disorders and the gut microbiome continues to be a source of exploration in modern research. The gut-brain axis is a biochemical signaling pathway thought to influence mood and brain functioning through a variety of mechanisms related to the immune system, inflammation modulation, and cellular metabolism. Microbiota-driven inflammatory responses and other alterations to the gut microbiome have been linked to psychiatric disorders and mood-related changes.
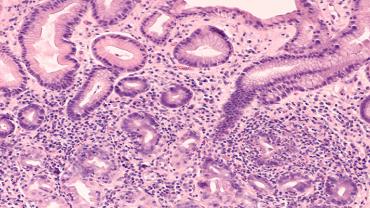
A recently published study aimed to correlate the symptom profiles of certain mood disorders with the composition of microbial DNA found in serum. The study consisted of 72 adult participants with previously diagnosed mood disorders. The researchers evaluated the composition of the microbiome by assaying microbe-derived extracellular vesicles (EVs) in serum. EVs are secretions from bacteria that contain genomic DNA fragments and can pass through the gastrointestinal mucus membrane. They have the potential to become a valuable means of assessing the composition of the gut microbiome because EVs are secretory. They may represent the metabolically active microbes in the microbiome. In addition, blood collection and analysis may be a logistically more feasible option.
The data collection regarding measurements of mood utilized the Hamilton Depression Rating Scale (HAM-D) and the Beck Anxiety Inventory (BAI). This also included 73 families and 137 genera from the gut microbiome in the analysis. The Bacterioidaceae family and Bacteroides genus were associated with better anxiety scores, and the Bacterioidaceae family (as a whole) was statistically significantly associated with better HAM-D scores.
The Desulfovibrionaceae family is known to produce hydrogen sulfide, which can pass through a cell membrane and inhibit butyrate oxidation, potentially causing changes in structure, function, and inflammation status. The Desulfovibrionaceae family DNA composition was positively associated with anxiety scores in this study. The authors postulate that hydrogen sulfide may be a link between anxiety severity and inflammation. Of note, the result of this study regarding Desulfovibrionaceae abundance was in direct opposition with current literature stating that the abundance of this family is lower in individuals with generalized anxiety disorder (GAD) than in healthy controls (HC), indicating that more research needs to be conducted and sample collection methods may require more validation. Similarly, the Clostridiales Family XIII was associated with higher BAI scores, which conflicts with previously reported studies that analyzed fecal samples. Some data reported in this study may conflict with modern literature, however, there is room for future studies to validate data collected from EV in serum.
Although more research needs to be conducted, this study shows promise that future analysis of the taxonomy of the gut microbiome may involve blood sampling. It also continues the contribution to research on the idea that the taxonomic structure of the gut microbiome may be correlated with mood disorders such as anxiety and depression. Supplementation and diets rich in probiotics may also support a healthy mood.
By Colleen Ambrose, ND, MAT