What effective therapy can possibly be better than your own body? So often, we are intent on finding solutions in traditional modalities that we forget about the strongest defense system known to man – the human immune system. Granted, the burdens of our toxic environments, adulterated foods, and stressful lifestyles have thwarted the power of this amazing system and left our bodies needing a support system, but what if we could re-harness that power and use it to support itself?
Natural killer cell immunotherapy is a step in the direction of harnessing the healing power of our own immune system. Nearly a decade ago, in 2008, natural killer cell immunotherapy was just newly being investigated as a potential treatment for malignancies. Today, it is being considered a new milestone for cancer therapy.
Natural killer cells (NKCs) are members of the lymphocyte family, but different from either B cells or T cells. They are born from the same lymphoid progenitor cell lines in the bone marrow as many other immune cells and once mature, they prefer to take up residence in lymphoid tissues as well as migrate to non-lymphoid tissue such as the lungs, liver, and peripheral blood.
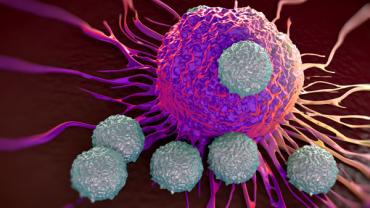
As their name suggests, their sole purpose is to kill cells (the abnormal ones, that is). Unlike the more common B and T cells, NKCs only make up about 10 to 15 percent of all circulating lymphocytes, but are among the most effective immune cells to monitor, recognize, and kill diseased cells without the need for prior sensitization or MHC restriction (self-recognizing signals that prevent the immune system from attacking). Instead, NKCs identify their targets through the integration of signals from activating and inhibitory receptors. Once the stressed, diseased, or abnormal cell is branded, NKCs begin the apoptotic process by interacting with the death receptor, secreting cytolytic granules, and/or producing chemokines and cytokines.
Often individuals with malignancies have impaired NKC function, which may involve incorrect signaling such as downregulation of activating receptors and/or upregulation of inhibitory receptors. Research has sought to find ways to enhance NKC quantity and activity as an adjunct to conventional therapies. Some trials have sought to use NKCs from a donor or directly from the patient. For example, in a phase I/II clinical trial assessing NKC immunotherapy on patients with metastatic gastrointestinal carcinoma, previously (but unsuccessfully) treated by a standard chemotherapy, NKCs were taken from a donor and transferred by hepatic intraarterial infusion to the subjects and resulted in a high expansion of T cells as well as an increase in cytokine activity. This study was among the first using NKC immunotherapy on solid tumors. In previous studies, NKCs did not display a good ability to infiltrate and eliminate large solid tumors. Instead, NKCs shine in their ability to eliminate cancer cells that enter the peripheral blood supply and therefore, are excellent defenses against metastasis, which accounts for 90 percent of the mortality associated with cancer. NKCs from donors have also shown high rates of success in patients with Acute Myeloid Leukemia.
Despite the potential therapeutic advantage of NKC immunotherapy, NKCs are still difficult to obtain from patients and donors. In response, current clinical trials are testing a iPSC-derived NK cell product in human subjects with advanced solid tumors. These NKCs are derived from an induced, genetically engineered pluripotent stem cell (iPSC), which eliminates the problem of donor compatibility and the time it takes to harvest your own NKCs. The trial is not scheduled to close until 2022 and although the use of genetically engineered stem cells will most assuredly raise multiple questions, it represents the latest trends in NKC immunotherapy. Nevertheless, it is a good reminder that some of the most therapeutically effective treatments are residing within the human body and when conventional therapies stall, it might be a good time to harness the power within.