In 2016 the U.S. Department of Health and Human Services rolled out the latest edition of their 2015-2020 Dietary Guidelines for Americans which created a shockwave effect. Something was missing in the new guidelines. Namely cholesterol limits disappeared. The new guidelines state “The Key Recommendation from the 2010 Dietary Guidelines to limit consumption of dietary cholesterol to 300 mg per day is not included in the 2015 edition… More research is needed regarding the dose-response relationship between dietary cholesterol and blood cholesterol levels. Adequate evidence is not available for a quantitative limit for dietary cholesterol specific to the Dietary Guidelines.” As traditionalists are shaking their heads and foreshadowing epidemics of cardiovascular disease non-conventionalists are celebrating victory. The new guidelines however are not completely sympathetic to the new change and are still quick to inform Americans that they “should eat as little dietary cholesterol as possible.” So although this reform is a success for practitioners who understand the requirements for adequate cholesterol the work is now cut out for us to begin disassembling the well-established fear of cholesterol from the minds of most Americans.
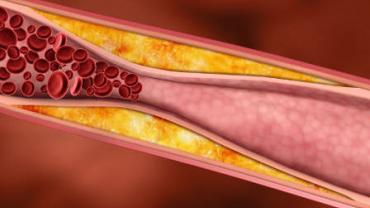
To a great degree the battle of dietary recommendations for cholesterol and other fats have hinged on the belief that serum cholesterol levels are a direct predictor of cardiovascular disease. Despite the broad awareness and even larger acceptance of this theory science still struggles to authenticate this claim. Dietary cholesterol and saturated fats do indeed influence serum cholesterol levels but is that truly a good predictor of cardiovascular risk? If history has any say in the matter decades of fat-free marketing food products and diet plans haven’t seemed to curtail the mortality rate and cardiovascular disease still remains the number one cause of death in this country. Dietary guidelines continue to push for an increase in omega-3 and omega-6 polyunsaturated fatty acids in place of saturated fats but again this advice is rooted in the so-called improvement in serum cholesterol ratios resulting from this shift in dietary fat even in the absence of cardiovascular improvements. We have even explored the effects of replacing saturated fats with carbohydrates on cardiovascular risk factors and not surprisingly that has not yielded positive results either. In fact replacing saturated fats with carbohydrates has worsened cardiovascular risks by increasing small dense low-density lipoprotein particles which are more indicative of cardiovascular events than large LDL particles which are produced by dietary saturated fats.
Slowly studies are emerging with fresh ideas pointing to oxidative stress inflammation and endothelial dysfunction – not hyperlipidemia – as major risk factors in cardiovascular disease. These same factors are associated with insulin resistance and type-2 diabetes making an obvious connection between the epidemic of deranged blood sugar levels and cardiovascular dysfunction – a.k.a. the phenomenon of metabolic syndrome. So why doesn’t the mainstream mindset focus on restricting inflammatory foods and processed foodstuffs that increase oxidative stress in favor of antioxidant-rich produce and fiber-filled legumes? Why has the focus persistently been upon cholesterol?
As alternative health care practitioners already know it is high time that the U.S. Department of Health and Human Services stop demonizing eggs and begin targeting some of the commodity crops for the cardiovascular mortality rates in this country. When 1032 participants were studied for 5 years in the prospective population-based Kuopio Ischaemic Heart Disease Risk Factor Study it was found that “egg or cholesterol intakes were not associated with increased CAD risk even in ApoE4 carriers (i.e. in highly susceptible individuals)” and yet recommendations to limit these items have been central to American dietary guidelines for decades. At the same time evidence points to dietary sugars as being a more influential factor on cardiometabolic risks independent of obesity. The OmniCarb study one of the largest studies “to test effects of high- versus low-GI diets in the context of moderate- and low-CHO diets” showed that higher total carbohydrate consumption rather than glycemic index contributed more negatively to cardiovascular risks. In an era and nation where carbohydrate and sugar consumption has extended beyond the ceiling level why isn’t the focus shifting to these food groups? Studies on the effects of carbohydrates on cardiovascular disease have been strangely stifled but to the keen observer this should not come as a surprise. After all grains and sugar are commodity foodstuffs heavily subsidized by the government so who would fund studies that would link these foodstuffs to America’s top cause of mortality?
While we can be thankful that the U.S. Department of Health and Human Services has finally taken the long overdue step of acknowledging that cholesterol and eggs are not a health trap and changing dietary guidelines accordingly it will take years to remove long held beliefs regarding cholesterol and cardiovascular disease. Nevertheless the next time a patient proudly exclaims that their doctor has given them a “clean bill of health” based on a standard lipid profile a prime opportunity stands waiting for you to re-educate one patient at a time.